Summary
- Medicare Advantage plans must prioritize digital strategies and member experiences to remain competitive and meet the needs of tech-savvy Baby Boomers aging into seniors.
- Member-centric enrollment and providing clear information on benefits creates a simplified consumer experience (CX).
- Digital health platforms and solutions should be accessible to the diverse Medicare Advantage population to ensure inclusivity.
In recent years, the significance of consumer experience (CX) in Medicare Advantage plans has grown exponentially. In fact, the weight placed on member experience in overall star ratings has increased from 1.5 in 2012 to a substantial 4 in 2020¹, and will only continue to increase in the coming years.
This, coupled with the rising number of tech-savvy Baby Boomers aging into Medicare Advantage plans, highlights the need for payers to embrace digital strategies and prioritize CX investments for these members. Developing a digital CX strategy for Medicare Advantage members not only gives payers a competitive edge in the market, but also provides tech-savvy seniors with more digital touchpoints and tools to empower them along their healthcare journey and ultimately leads to better business outcomes for health plans.
The Tech Boom
The influx of Baby Boomers entering Medicare presents a significant opportunity for Medicare Advantage plans. The next wave of high-value, tech-savvy Baby Boomers are eager to search for available plans, providers and prescriptions, compare prices and star ratings, and make informed purchasing decisions as they would on their favorite online retailer sites. Empowering these members requires providing them with the necessary digital tools and resources that allows them to understand their plan benefits, coordinate care and communicate with their plan.
According to the Pew Research Center, 94% of seniors own smartphones in 2024²
Simplify & amplify: CX strategies in Medicare Advantage Plans
By prioritizing member-centric approaches and leveraging technology, health plans can foster stronger relationships, increase Medicare Advantage member experience, and ultimately thrive in the market. Simplifying enrollment and onboarding, providing personalized omnichannel communication, improving care coordination, and enhancing digital solutions are key strategies for achieving this goal.
The power of simplicity
Enrolling in a Medicare Advantage plan can often be overwhelming for members. To alleviate this, the focus should be on simplifying the process and proactively providing concise information about coverage, benefits, and care information in one central place.
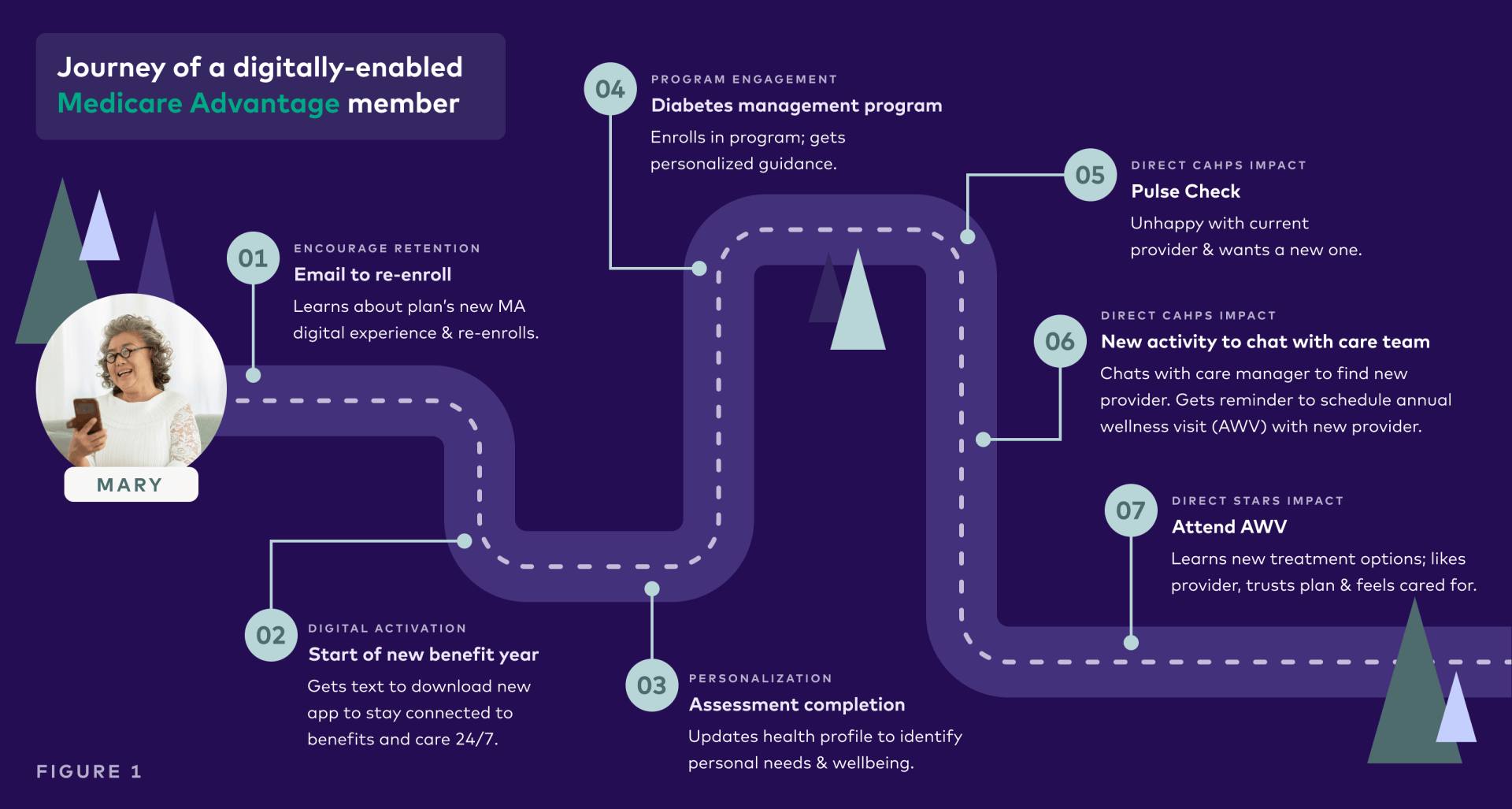
Let’s take a look at a hypothetical Medicare Advantage plan member, Mary. She is 67 years old and is looking for more support to help her manage her type 2 diabetes and improve her overall health. During the re-enrollment period, she receives an email from her health plan about re-enrolling for another year. Upon enrollment, she receives a text message to download her plan’s new digital app. This digital app offers her a single place where she can access all her benefits and wellness information (See Figure 1). The process was proactive and simple for Mary, and provided a positive experience during a crucial stage in the member journey that can have a direct impact on CAHPS and NPS.
That personal touch
Medicare Advantage members exhibit a wide range of diversity, nuances, and unique health drivers, differentiating them not only from traditional commercial plan members but also from one another. Understanding your Medicare Advantage member is crucial for delivering personalized and relevant messaging to move them along their healthcare journey. By leveraging data and analytics, health plans can gain insights into member demographics, preferences, and health needs. This information can be used to tailor member communications and interactions and ultimately improves the Medicare Advantage member experience.
Let’s go back to Mary. After she is onboarded onto her health plan’s new digital app and provides her communication preferences, she begins to create her digital profile by answering important questions about her health goals and personal needs. This first party data, along with information that she has given the app access to like her fitness trackers, glucose monitor and more, allows her health plan to collect relevant data about Mary that can be used to personalize her experience. The data collected about her, including information on her comorbidities, triggers a diabetes wellness program that she can enroll in to better manage her condition. Placing the member at the center and using data to provide relevant touchpoints in their journey helps build stronger relationships and fosters stronger engagement.
Bridging the gap
Medicare Advantage members often have multiple chronic conditions and complex care needs, therefore, effective care coordination becomes essential to manage their healthcare journey. Without proper care coordination, efficient communication and information sharing among care teams, members and their families, there is a risk of a fragmented and frustrating experience.
Mary, for example, indicated that she wanted better support in managing her type 2 diabetes. Having a chronic condition, it is important for her health plan to proactively support her with ways to easily get in touch with her PCP, schedule appointments, provide important reminders and provide resources and information on her condition. Prompting regular pulse checks in the app allows her plan to also gain real-time feedback and proactively address concerns. By facilitating communication between Mary and her care team, offering both physical and digital touchpoints and resolving challenges based on her feedback, reduces communication gaps and leaves Mary feeling empowered and cared for by her health plan which will reflect positively for the health plan in CAHPS and NPS.
Designing for inclusivity
The Medicare Advantage population encompasses a diverse range of individuals, including those with varying physical, sensory, and cognitive abilities. With the increasing use of technology in healthcare, it is essential that Medicare Advantage health plans ensure their digital interfaces, such as websites and mobile apps, are accessible and inclusive.
As plans seek to enhance digital tools for Medicare Advantage members, they need to be mindful of making assumptions on what features are necessary or helpful. “We all have to understand that we live with inherent bias. And we have to constantly check those assumptions. We have to make sure that the tools that are implemented allow access for as many people as possible. Tools should be created by a diverse group of people and tested by an equally diverse group of people.” said Jess Tschirki, VP of Design at League
By adopting inclusive design principles, health plans can create experiences that accommodate the unique needs and preferences of all members.
Seize the Advantage
Nearly 31 million Americans are enrolled in Medicare Advantage plans, with thousands of new members enrolling every day³. Incentivized by strict regulations, consistent growth and rising consumer expectations these plans face heightened pressures to innovate.
By adopting technology-driven solutions, implementing best practices, and actively engaging members through CX technology and digital support tools, health plans can enhance the consumer experience, improve member satisfaction, increase star ratings and ultimately thrive in this competitive market.
To gain more insights from leading health plans on how to improve member experiences and deliver business value through CX transformation, download our latest whitepaper with Becker’s, “Transforming the member experience to unlock business value.”
New research from Becker’s
Gain actionable insights on how to measure the value of your digital CX investments and how to use these investments to win in today’s highly competitive market.
Sources
¹The Impact of Proposed Changes to the CMS Star Ratings Program, Carenet Health
²Demographics of Mobile Device Ownership and Adoption, Pew Research Center
³CMS data: Medicare Advantage enrollment now more than 31M, Fierce Healthcare
